INTRODUCTION
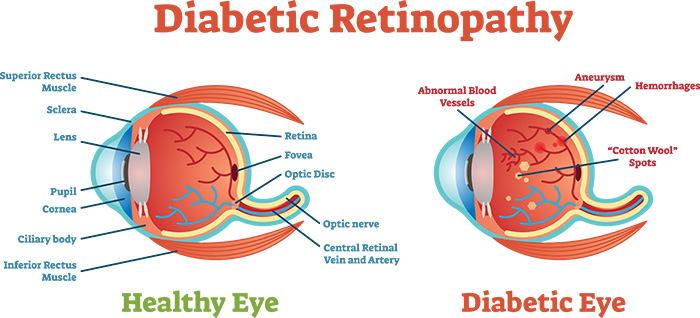
Diabetic retinopathy is a diabetes complication that affects eyes. It's caused by damage to the blood vessels of the light-sensitive tissue at the back of the eye (retina). These blood vessels can swell and leak. Or they can close, stopping blood from passing through. Sometimes abnormal new blood vessels grow on the retina. All of these changes can steal your vision. At first, diabetic retinopathy may cause no symptoms or only mild vision problems. Eventually, it can cause blindness.
The condition can develop in anyone who has type 1 or type 2 diabetes. The longer you have diabetes and the less controlled your blood sugar is, the more likely you are to develop this eye complication.
TYPES
There are two types of diabetic retinopathy:
∑ Early diabetic retinopathy. In this more common form ó called nonproliferative diabetic retinopathy (NPDR) ó new blood vessels aren't growing (proliferating).
When you have NPDR, the walls of the blood vessels in your retina weaken. Tiny bulges (microaneurysms) protrude from the vessel walls of the smaller vessels, sometimes leaking fluid and blood into the retina. Larger retinal vessels can begin to dilate and become irregular in diameter, as well. NPDR can progress from mild to severe, as more blood vessels become blocked. Also with NPDR, blood vessels in the retina can close off. This is called macular ischemia. When that happens, blood cannot reach the macula. Sometimes tiny particles called exudates can form in the retina. These can affect your vision too.
Nerve fibers in the retina may begin to swell. Sometimes the central part of the retina (macula) begins to swell (macular edema), a condition that requires treatment.
∑ Advanced diabetic retinopathy also called PDR (proliferative diabetic retinopathy)- Diabetic retinopathy can progress to this more severe type, known as proliferative diabetic retinopathy. In this type, damaged blood vessels close off, causing the growth of new, abnormal blood vessels in the retina, and can leak into the clear, jelly-like substance that fills the center of your eye (vitreous).
Eventually, scar tissue stimulated by the growth of new blood vessels may cause the retina to detach from the back of your eye. If the new blood vessels interfere with the normal flow of fluid out of the eye, pressure may build up in the eyeball. This can damage the nerve that carries images from your eye to your brain (optic nerve), resulting in glaucoma.
SYMPTOMS
You can have diabetic retinopathy and not know it. This is because it often has no symptoms in its early stages. As diabetic retinopathy gets worse, you will notice symptoms such as:
- seeing an increasing number of floaters,
- having blurry vision,
- having vision that changes sometimes from blurry to clear,
- seeing blank or dark areas in your field of vision,
- having poor night vision, and
- noticing colors appear faded or washed out losing vision.
Diabetic retinopathy symptoms usually affect both eyes.
CAUSES
Over time, too much sugar in your blood can lead to the blockage of the tiny blood vessels that nourish the retina, cutting off its blood supply. As a result, the eye attempts to grow new blood vessels. But these new blood vessels don't develop properly and can leak easily.
COMPLICATIONS
Possible complications associated with diabetic retinopathy include the following:
Vitreous hemorrhage: A newly formed blood vessel leaks into the vitreous gel that fills the eye, stopping light from reaching the retina. Symptoms include loss of vision and sensitivity to light, or floaters in milder cases. This complication can resolve itself if the retina remains undamaged.
Detached retina: Scar tissue can pull the retina away from the back of the eye. This usually causes the appearance of floating spots in the individualís field of vision, flashes of light, and severe vision loss. A detached retina presents a significant risk of total vision loss if left untreated.
Glaucoma: The normal flow of fluid in the eye may become blocked as new blood vessels form. The blockage causes a buildup of ocular pressure, or pressure in the eye, increasing the risk of optic nerve damage and vision loss.
Blindness. Eventually, diabetic retinopathy, glaucoma or both can lead to complete vision loss.
RISK FACTORS
Anyone who has diabetes can develop diabetic retinopathy. Risk of developing the eye condition can increase as a result of:
∑ Duration of diabetes ó the longer you have diabetes, the greater your risk of developing diabetic retinopathy
∑ Poor control of your blood sugar level
∑ High blood pressure
∑ High cholesterol
∑ Pregnancy
∑ Tobacco use
∑ Being African-American, Hispanic or Native American
PREVENTION
You can't always prevent diabetic retinopathy. However, regular eye exams, good control of your blood sugar and blood pressure, and early intervention for vision problems can help prevent severe vision loss.
If you have diabetes, reduce your risk of getting diabetic retinopathy by doing the following:
∑ Manage your diabetes. Make healthy eating and physical activity part of your daily routine. Try to get at least 150 minutes of moderate aerobic activity, such as walking, each week. Take oral diabetes medications or insulin as directed.
∑ Monitor your blood sugar level. You may need to check and record your blood sugar level several times a day ó more-frequent measurements may be required if you're ill or under stress. Ask your doctor how often you need to test your blood sugar.
∑ Ask your doctor about a glycosylated hemoglobin test. The glycosylated hemoglobin test, or hemoglobin A1C test, reflects your average blood sugar level for the two- to three-month period before the test. For most people, the A1C goal is to be under 7 percent.
∑ Keep your blood pressure and cholesterol under control. Eating healthy foods, exercising regularly and losing excess weight can help. Sometimes medication is needed, too.
∑ If you smoke or use other types of tobacco, ask your doctor to help you quit. Smoking increases your risk of various diabetes complications, including diabetic retinopathy.
∑ Pay attention to vision changes. Contact your eye doctor right away if you experience sudden vision changes or your vision becomes blurry, spotty or hazy.
Remember, diabetes doesn't necessarily lead to vision loss. Taking an active role in diabetes management can go a long way toward preventing complications.
Diabetic retinopathy generally starts without any noticeable change in vision. However, an ophthalmologist, or eye specialist, can detect the signs.
It is crucial for people with diabetes to have an eye examination at least once or twice annually, or when recommended by a physician.
The following methods are commonly used to diagnose diabetic retinopathy:
Dilated eye exam
The doctor administers drops into the patientís eyes. These drops dilate the pupils and allow the doctor to view the inside of the eye in a more detailed way.
Photographs are taken of the interior of the eye. During the eye examination, the doctor can detect the presence of:
- abnormalities in the blood vessels, optic nerve, or retina
- cataracts
- changes in eye pressure or overall vision
- new blood vessels
- retinal detachment
- scar tissue
These drops may sting, and the bright lights of the photographs can startle the person receiving the test. In high-risk individuals, the eye drops may cause an increase in ocular pressure.
Fluorescein angiography
Drops are used to dilate the pupils, and a special dye called fluorescein is injected into a vein in the patientís arm. Pictures are taken as the dye circulates through the eyes. The dye may leak into the retina or stain the blood vessels if the blood vessels are abnormal.
This test can determine which blood vessels are blocked, leaking fluid, or broken down. Any laser treatments can then be accurately guided. For around 24 hours after the test, the skin may turn yellowish, and urine dark orange, as the dye exits the body.
Optical coherence tomography (OCT)
This noninvasive imaging scan provides high-resolution cross-sectional images of the retina, revealing its thickness. After any treatments, scans may be used later to check how effective treatment has been.
OCT is similar to ultrasound testing but uses light rather than sound to produce images. The scan can also detect diseases of the optic nerve.
TREATMENT
Treating DR depends on several factors, including the severity and type of DR, and how the person with DR has responded to previous treatments.
With NPDR, a doctor may decide to monitor the personís eyes closely without intervening. This is known as watchful waiting.
Individuals will need to work with their doctor to control diabetes. Good blood sugar control can significantly slow the development of DR.
In most cases of PDR, the patient will require immediate surgical treatment. The following options are available:
Focal laser treatment, or photocoagulation
The procedure is carried out in a doctorís office or an eye clinic. Targeted laser burns seal the leaks from abnormal blood vessels. Photocoagulation can either stop or slow down the leakage of blood and buildup of fluid in the eye.
People will usually experience blurry vision for 24 hours following focal laser treatment. Small spots may appear in the visual field for a few weeks after the procedure.
Scatter laser treatment, or pan-retinal photocoagulation
Scattered laser burns are applied to the areas of the retina away from the macula, normally over the course of two or three sessions. The macula is the area at the center of the retina in which vision is strongest.
The laser burns cause abnormal new blood vessels to shrink and scar. Most patients require two or three sessions for the best results.
Individuals may have blurry vision for 24 hours following the procedure, and there may be some loss of night vision or peripheral vision.
Vitrectomy
This involves the removal some of the vitreous from within the eyeball. The surgeon replaces the clouded gel with a clear liquid or gas. The body will eventually absorb the gas or liquid. This will create new vitreous to replace the clouded gel that has been removed.
Any blood in the vitreous and scar tissue that may be pulling on the retina is removed. This procedure is performed in a hospital under general or local anesthetic.
The retina may also be strengthened and held in position with tiny clamps.
After surgery, the patient may have to wear an eye patch to gradually regain use of their eye, which can tire after a vitrectomy.
If gas was used to replace the removed gel, the patient should not travel by plane until all gas has been absorbed into the body. The surgeon will tell the patient how long this should take. Most patients will have blurry vision for a few weeks after surgery. It can take several months for normal vision to return.
Surgery is not a cure for diabetic retinopathy. However, it may stop or slow the progression of symptoms. Diabetes is a long-term condition, and subsequent retinal damage and vision loss may still occur despite treatment.