INTRODUCTION
Muscular Dystrophy (MD) is a group of neuromuscular genetic disorders that cause muscle weakness and overall loss of muscle mass. MD is a progressive condition; meaning that it gets worse with the passage of time. Muscular Dystrophy is considered as a disability in many countries including the USA (under Americans with Disabilities Act) and India (under Rights of Persons with Disabilities Act). Some types of MD eventually affect the heart or the muscles used for breathing, at which point the condition becomes life-threatening. At present, there is no cure available for Muscular Dystrophy.
TYPES OF MUSCULAR DYSTROPHY
1. Myotonic (also called MMD or Steinert’s disease)
2. Duchenne
3. Becker
4. Limb-girdle
5. Facioscapulohumeral
6. Congenital
7. Oculopharyngeal
8. Distal
9. Emery-Dreifuss

Duchenne muscular dystrophy
As a result of the way it's inherited, Duchenne MD mostly affects boys. Girls can occasionally be affected, although the condition tends to be milder.
Children with Duchenne MD usually start to have noticeable symptoms between 1 and 3 years of age. The muscles around their pelvis and thighs tend to be affected first and often appear bulkier than normal.
A child with Duchenne MD may:
- have difficulty walking, running or jumping
- have difficulty standing up
- learn to speak later than usual
- be unable to climb the stairs without support
- have behavioural or learning difficulties
Children with Duchenne MD may need a wheelchair by the time they're 12 years old, as their muscles weaken and they lose the ability to walk. They can also develop scoliosis, where the spine begins to curve sideways. This can lead to one shoulder or hip being higher than the other.
By their mid-teens, some people with Duchenne MD will develop dilated cardiomyopathy. This condition affects the heart muscles, causing the heart's chambers to enlarge and the walls to get thinner.
By their late-teens or early 20s, people with Duchenne MD may start to have breathing problems. The condition can also affect the intercostal muscles (muscle tissue between the ribs) and the diaphragm (the large, thin sheet of muscle between the chest and abdomen).
Once the heart and respiratory muscles are damaged, Duchenne MD becomes life-threatening. With medical care, most people with Duchenne MD die from heart or respiratory failure before or during their 30s.
Myotonic dystrophy
As with other types of muscular dystrophy, myotonic dystrophy involves progressive muscle weakness and muscle wasting. However, it's often the smaller muscles that are affected first, such as those in the face, jaw and neck.
Myotonic dystrophy can appear at any time between birth and old age. It affects the same number of men and women.
As well as muscle weakness and wasting, symptoms can include:
- muscle stiffness (myotonia)
- clouding of the lens in the eye (cataracts)
- excessive sleeping or sleepiness
- difficulty swallowing
- behavioural and learning problems in children
- a slow and irregular heartbeat (cardiac arrhythmia)
Myotonic dystrophy is highly variable and often gets worse very slowly, with little change over long periods of time. However, it can become more severe as it's passed down through the generations.
Some people with myotonic dystrophy may never have a significant disability, although their heart rate will need to be monitored for abnormalities. This is because there's a risk of the electrical impulses that control the heartbeat travelling too slowly through the heart. In some people, the condition can also cause cataracts to develop at a younger age than usual.
Life expectancy for people with myotonic dystrophy can vary considerably. Many people have a normal life expectancy, but people with the more severe congenital form (present from birth) may die while still a newborn baby, or only survive for a few years.
Some people who first develop symptoms as a child or teenager may also have a shortened life expectancy. Most deaths related to myotonic dystrophy are related to pneumonia, breathing problems or heart problems.
If you have myotonic dystrophy, it's important that you're well informed about your condition, and that you tell any healthcare professionals you see that you have it. Myotonic dystrophy can cause difficulties with general anaesthetics and childbirth.
Facioscapulohumeral muscular dystrophy
Facioscapulohumeral MD can affect both men and women. It tends to affect men slightly more than women, although the reason for this is unclear. Men also tend to be affected earlier and more severely.
About 1 in 3 people with facioscapulohumeral MD are unaware of any symptoms until well into adulthood. Others develop problems in early childhood. The condition tends to progress slowly.
Signs in your child may include:
- sleeping with their eyes slightly open
- an inability to squeeze their eyes tightly shut
- an inability to purse their lips – for example, to blow up balloons
Teenagers or adults may have shoulder aches, rounded shoulders or thin upper arms. As the condition progresses, it usually affects the muscles in the:
- face (facio)
- shoulders (scapula)
- upper arms (humeral)
- upper back
- calves
Around half of all people with facioscapulohumeral MD develop weakness in their leg muscles, and 1 or 2 in every 10 people with the condition will eventually need a wheelchair.
Facioscapulohumeral MD can develop unevenly, so the muscles on one side of the body may be affected more than the other. As the condition progresses slowly, it doesn't usually shorten life expectancy.
Distal
This group of rare diseases affects adult men and women. It causes weakness and wasting of the distal muscles (those farthest from the center) of the forearms, hands, lower legs, and feet. It is generally less severe, progresses more slowly, and affects fewer muscles than other forms of muscular dystrophy. Distal muscular dystrophy is also called distal myopathy. It affects the muscles in your:
- forearms
- hands
- calves
- feet
It may also affect your respiratory system and heart muscles. The symptoms tend to progress slowly and include a loss of fine motor skills and difficulty walking. Most people, both male and female, are diagnosed with distal muscular dystrophy between the ages of 40 and 60.
Becker muscular dystrophy
Like Duchenne MD, Becker MD mostly affects boys. Becker MD also affects similar areas of the body to Duchenne MD, although the symptoms tend to be less severe.
Symptoms of Becker MD usually begin in childhood, but they're often relatively mild at this point. For example, a child with the condition may:
- learn to walk later than usual
- have muscle cramps when exercising
- struggle with sports at school
During late childhood or early adulthood, people with Becker MD often find they have difficulty running, walking quickly and climbing stairs. As they get older, they may also find lifting objects above waist height difficult.
Most people with Becker MD will be able to walk into their 40s and 50s but often find they need to use a wheelchair as their condition progresses.
If you have Becker MD, you're also at risk of developing dilated cardiomyopathy and breathing problems. However, Becker MD progresses at a slower rate than Duchenne MD, and those with the condition often have a normal lifespan.
Congenital
Congenital means present at birth. Congenital muscular dystrophies progress slowly and affect males and females. The two forms that have been identified -- Fukuyama and congenital muscular dystrophy with myosin deficiency -- cause muscle weakness at birth or in the first few months of life, along with severe and early contractures (shortening or shrinking of muscles that causes joint problems). Fukuyama congenital muscular dystrophy causes abnormalities in the brain and often seizures. Symptoms vary and may include:
- muscle weakness
- poor motor control
- inability to sit or stand without support
- scoliosis
- foot deformities
- trouble swallowing
- respiratory problems
- vision problems
- speech problems
- intellectual impairment
While symptoms vary from mild to severe, the majority of people with congenital muscular dystrophy are unable to sit or stand without help. The lifespan of someone with this type also varies, depending on the symptoms. Some people with congenital muscular dystrophy die in infancy while others live until adulthood.
Limb-girdle muscular dystrophy
Limb-girdle MD refers to a number of related conditions that cause weakness in the big muscle groups at the base of the arms and legs (around the shoulders and hips).
The first symptoms are often mobility problems affecting the hip girdle. It then progresses to the shoulder girdle ("girdle" means the bones around the shoulder or hip).
Symptoms of limb-girdle MD usually begin in late childhood or early adulthood, although the condition can affect people younger or older than this, depending on the specific type. Males and females are equally affected.
If you have limb-girdle MD, you may experience:
- muscle weakness in your hips, thighs and arms
- loss of muscle mass in the affected areas
- back pain
- heart palpitations or irregular heartbeats
The muscle weakness will create problems such as difficulty lifting objects, running or getting out of a low seat.
How quickly limb-girdle MD progresses depends on the specific type. Many types get worse slowly, whereas others can develop more rapidly.
Oculopharyngeal muscular dystrophy
In oculopharyngeal MD, symptoms aren't usually apparent until a person is around 50 years old. It affects the muscles in the eyes (ocular) and the throat (pharyngeal).
Symptoms of oculopharyngeal MD can include:
- droopy eyelids
- difficulty swallowing (dysphagia)
- progressive restriction of eye movement as the eye muscles become affected
- limb weakness around the shoulders and hips
As the eyelids droop, they can cover the eyes and impair vision. It's also possible to develop double vision.
Dysphagia can eventually make it difficult to swallow solid foods, liquids and even small amounts of saliva. This can lead to chest infections if food and drink is accidentally swallowed the "wrong way" into the lungs. However, with treatment to manage the symptoms, a person's life expectancy isn't usually altered.
Emery-Dreifuss muscular dystrophy
People with Emery-Dreifuss MD often begin to develop symptoms during childhood or adolescence.
In the early stages, people with the condition usually develop muscle contractures (where the muscles and tendons become shortened and tightened, limiting the range of movement at nearby joints).
Areas commonly affected by muscle contractures include the arms, neck and feet. This means that people with Emery-Dreifuss MD may have difficulty straightening their elbows or bending their neck forward, for example.
Like all types of MD, Emery-Dreifuss MD also causes progressive muscle weakness, usually beginning in the shoulders, upper arms and lower legs. This can make it difficult to lift heavy objects or raise your arms above your head, and you may have an increased tendency to trip over things.
Later on, the hip and thigh muscles become weaker, making activities such as walking up stairs difficult. People with Emery-Dreifuss MD will often eventually require a wheelchair, as they become unable to walk.
Emery-Dreifuss MD can also affect the heart's electrical signals, causing heart block. This can result in people with the condition developing an abnormally slow heartbeat and palpitations, which can lead to episodes of lightheadedness or fainting. The slow heartbeat can often be treated successfully with an implanted pacemaker.
Due to the risk of serious heart and respiratory problems, someone with Emery-Dreifuss MD will often have a shortened life expectancy. However, most people with the condition live until at least middle age.
CAUSES
In most cases, muscular dystrophy (MD) runs in families. It usually develops after inheriting a faulty gene from one or both parents.
MD is caused by mutations (alterations) in the genes responsible for healthy muscle structure and function. The mutations mean that the cells that should maintain your muscles can no longer fulfil this role, leading to muscle weakness and progressive disability.
Inheriting muscular dystrophy
You have two copies of every gene (with the exception of the sex chromosomes). You inherit a copy from one parent, and the other copy from the other parent. If one or both of your parents has a mutated gene that causes MD, it can be passed on to you.
Depending on the specific type of MD, the condition can be a:
- recessive inherited disorder
- dominant inherited disorder
- sex-linked (X-linked) disorder
In a few cases, the genetic mutation that causes MD can also develop as a new event in the family. This is known as a spontaneous mutation. Examples include:
A recessive inherited disorder
If you have a recessive inherited disorder, it means you've inherited an altered version of the gene that causes the condition from both of your parents (both your copies of the gene are altered).
If a child only inherits an altered version of the gene from one parent, they'll become a carrier of the condition. This means they're not affected, but there's a chance that any children they have will be if their partner is also a carrier.
If both parents carry an altered version of the gene that causes the condition, there's a:
- 1 in 4 chance their child will have MD
- 1 in 4 chance their child will be healthy but carry the mother's faulty gene
- 1 in 4 chance their child will be healthy but carry the father's faulty gene
- 1 in 4 chance their child will be healthy (won't inherit any mutated genes)
Some types of limb-girdle MD are inherited in this way.
A dominant inherited disorder
A dominant inherited disorder means you only need to inherit the mutated gene from one parent to be affected.
This means that if you have a child with an unaffected partner, there's still a 50% chance of your child developing the condition.
Types of MD inherited in this way include myotonic dystrophy, facioscapulohumeral MD, oculopharyngeal MD and some types of limb-girdle MD.
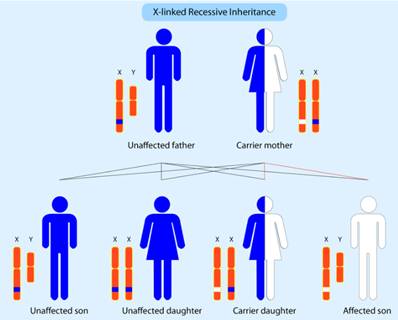
A sex-linked (X-linked) disorder
Chromosomes are long, threadlike structures of DNA. A male has one X and one Y sex chromosome, and a female has two X chromosomes.
A sex-linked disorder is caused by a mutation in a gene on the X chromosome. As males only have one copy of each gene on the X chromosome, they'll be affected if one of those genes is mutated.
As females have two copies of the X chromosome, they're less likely to develop an X-linked condition, because the normal copy of the chromosome can usually cover for (mask) the altered version.
Females can still be affected by X-linked disorders, but the condition is usually less severe than when the gene alteration is present in an affected male.
Types of MD inherited in this way include Duchenne MD and Becker MD, which is why these conditions are more common and more severe in males.
Spontaneous gene mutations
Spontaneous gene mutations can occasionally cause MD. This is where the genes mutate for no apparent reason, changing the way the cells function. Spontaneous gene mutations can cause MD to develop in people who don't have a family history of the condition.
Another way a child with no family history can be affected is when the condition is recessive. The gene mutations may have been present on both sides of the family for many generations but may not have affected anyone until a child inherited a copy of the altered gene from both parents.
- Enzyme assay: Damaged muscles produce creatine kinase (CK). Elevated levels of CK in the absence of other types of muscle damage could suggest muscular dystrophy.
- Genetic testing: As genetic mutations are known to occur in muscular dystrophy, these changes can be screened for.
- Heart monitoring: Electrocardiography and echocardiograms can detect changes in the musculature of the heart. This is especially useful for the diagnosis of myotonic muscular dystrophy.
- Lung monitoring: Checking lung function can give additional evidence.
- Electromyography: A needle is placed into the muscle to measure the electrical activity. The results can show signs of muscle disease.
- Biopsy: Removing a portion of muscle and examining it under a microscope can show the tell-tale signs of muscular dystrophy.
TREATMENT
Although there's no cure for any form of muscular dystrophy, treatment for some forms of the disease can help extend the time a person with the disease can remain mobile and help with heart and lung muscle strength. Trials of new therapies are ongoing.
People with muscular dystrophy should be monitored throughout their lives. Their care team should include a neurologist with expertise in neuromuscular diseases, a physical medicine and rehabilitation specialist, and physical and occupational therapists.
Some people might also need a lung specialist (pulmonologist), a heart specialist (cardiologist, a sleep specialist, a specialist in the endocrine system (endocrinologist), an orthopedic surgeon and other specialists.
Treatment options include medications, physical and occupational therapy, and surgical and other procedures. Ongoing assessments of walking, swallowing, breathing and hand function enable the treatment team to adjust treatments as the disease progresses.
Medications
Your doctor might recommend:
· Corticosteroids, such as prednisone and deflazacort (Emflaza), which can help muscle strength and delay the progression of certain types of muscular dystrophy. But prolonged use of these types of drugs can cause weight gain and weakened bones, increasing fracture risk.
· Newer drugs include eteplirsen (Exondys 51), the first medication to be approved by the Food and Drug Administration (FDA) specifically to treat some people with Duchenne muscular dystrophy. It was conditionally approved in 2016.
In 2019, the FDA approved golodirsen (Vyondys 53) for treatment of some people with Duchenne dystrophy who have a certain genetic mutation.
· Heart medications, such as angiotensin-converting enzyme (ACE) inhibitors or beta blockers, if muscular dystrophy damages the heart.
Therapy
Several types of therapy and assistive devices can improve the quality and sometimes the length of life in people who have muscular dystrophy. Examples include:
· Range-of-motion and stretching exercises. Muscular dystrophy can restrict the flexibility and mobility of joints. Limbs often draw inward and become fixed in that position. Range-of-motion exercises can help to keep joints as flexible as possible.
· Exercise. Low-impact aerobic exercise, such as walking and swimming, can help maintain strength, mobility and general health. Some types of strengthening exercises also might be helpful. But it's important to talk to your doctor first because some types of exercise might be harmful.
· Braces. Braces can help keep muscles and tendons stretched and flexible, slowing the progression of contractures. Braces can also aid mobility and function by providing support for weakened muscles.
· Mobility aids. Canes, walkers and wheelchairs can help maintain mobility and independence.
· Breathing assistance. As respiratory muscles weaken, a sleep apnea device might help improve oxygen delivery during the night. Some people with severe muscular dystrophy need to use a machine that forces air in and out of their lungs (ventilator).
Surgery
Surgery might be needed to correct contractures or a spinal curvature that could eventually make breathing more difficult. Heart function may be improved with a pacemaker or other cardiac device.
Preventing respiratory infections
Respiratory infections can become a problem in muscular dystrophy. So, it's important to be vaccinated for pneumonia and to keep up to date with influenza shots. Try to avoid contact with children or adults who have an obvious infection.