INTRODUCTION
Trachoma is the leading infectious cause of blindness worldwide. It is caused by an obligate intracellular bacterium called Chlamydia trachomatis. The infection is transmitted by direct or indirect transfer of eye and nose discharges of infected people, particularly young children who harbour the principal reservoir of infection. These discharges can be spread by particular species of flies. It can also be passed on by handling infected items, such as handkerchiefs.
At first, trachoma may cause mild itching and irritation of your eyes and eyelids. Then you may notice swollen eyelids and pus draining from the eyes. Untreated trachoma can lead to blindness.
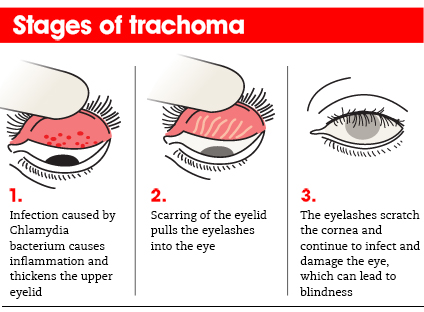
STAGES OF TRACHOMA
The World Health Organization has identified five stages in the development of trachoma:
· Inflammation — follicular. The infection is just beginning in this stage. Five or more follicles — small bumps that contain lymphocytes, a type of white blood cell — are visible with magnification on the inner surface of your upper eyelid (conjunctiva).
· Inflammation — intense. In this stage, your eye is now highly infectious and becomes irritated, with a thickening or swelling of the upper eyelid.
· Eyelid scarring. Repeated infections lead to scarring of the inner eyelid. The scars often appear as white lines when examined with magnification. Your eyelid may become distorted and may turn in (entropion).
· Ingrown eyelashes (trichiasis). The scarred inner lining of your eyelid continues to deform, causing your lashes to turn in so that they rub on and scratch the transparent outer surface of your eye (cornea).
· Corneal clouding. The cornea becomes affected by an inflammation that is most commonly seen under your upper lid. Continual inflammation compounded by scratching from the in-turned lashes leads to clouding of the cornea.
All the signs of trachoma are more severe in your upper lid than in your lower lid. With advanced scarring, your upper lid may show a thick line.
In addition, the lubricating glandular tissue in your lids — including the tear-producing glands (lacrimal glands) — can be affected. This can lead to extreme dryness, aggravating the problem even more.
GRADING:
The WHO grading system for trachoma classifies the disease in 5 grades:
· Trachomatous Inflammation – Follicular (TF) - which mostly requires topical treatment.
· Trachomatous Inflammation – Intense (TI) - during which topical and systemic treatments are considered.
· Trachomatous Scarring (TS) - when scars are visible as in the tarsal conjunctiva and which may obscure tarsal blood vessels.
· Trachomatous Trichiasis (TT) - when an individual is referred for eyelid surgery; and
· Corneal Opacity - a stage during which a person is irreversibly blind.
CLINICAL FINDINGS
The clinical manifestations of trachoma can be divided into findings associated with active disease and those associated with repeat infections.
Active Disease:
· Follicular Conjunctivitis: Follicles are dome-shaped collections of lympoid cells. The center of the follicle is avascular and has blood vessels that surround the round base. These appear as yellow-white elevations and are prominent on the everted upper eyelid in trachoma. Large conjunctival follicles located at the upper margin of the cornea may leave depressions known as 'Herbert's pits' which are pathognomonic for trachoma.
· Papillary Hypertrophy: engorgement of small vessels with edema that can obscure deep tarsal vessels
· Corneal Pannus: vascularization of the upper cornea.
Repeat Infection and Inflammation:
· Conjunctival Scarring: White bands or lines that represent fibrosis
· Cicatricial Entropion and Trichiasis: Fibrotic scar tissue contraction causes the eyelid turning inward and lashes touching the eyeball.
· Corneal Opacification: secondary to repeat corneal irritation from inward turning eyelashes
SYMPTOMS
Signs and symptoms of trachoma usually affect both eyes and may include:
· Mild itching and irritation of the eyes and eyelids
· Discharge from the eyes containing mucus or pus
· Eyelid swelling
· Light sensitivity (photophobia)
· Eye pain
Young children are particularly susceptible to infection. But the disease progresses slowly, and the more painful symptoms may not emerge until adulthood.
CAUSES
Trachoma is caused by certain subtypes of Chlamydia trachomatis, a bacterium that can also cause the sexually transmitted infection chlamydia.
Trachoma spreads through contact with discharge from the eyes or nose of an infected person. Hands, clothing, towels and insects can all be routes for transmission. In developing countries, eye-seeking flies also are a means of transmission.
RISK FACTORS
Factors that increase your risk of contracting trachoma include:
· Poverty. Trachoma is primarily a disease of extremely poor populations in developing countries.
· Crowded living conditions. People living in close contact are at greater risk of spreading infection.
· Poor sanitation. Poor sanitary conditions and lack of hygiene, such as unclean faces or hands, help spread the disease.
· Age. In areas where the disease is active, it's most common in children ages 4 to 6.
· Sex. In some areas, women's rate of contracting the disease is two to six times higher than that of men.
· Flies. People living in areas with problems controlling the fly population may be more susceptible to infection.
· Lack of latrines. Populations without access to working latrines — a type of communal toilet — have a higher incidence of the disease.
PREVENTION
If you've been treated for trachoma with antibiotics or surgery, reinfection is always a concern. For your protection and for the safety of others, be sure that family members or others you live with are screened and, if necessary, treated for trachoma.
Trachoma can occur worldwide but is more common in the Middle East, North Africa, sub-Saharan Africa, and areas of southern Asia and China. When in regions where trachoma is common, take extra care in practicing good hygiene, which can help prevent infection.
Proper hygiene practices include:
· Face washing and hand-washing. Keeping faces clean may help break the cycle of reinfection.
· Controlling flies. Reducing fly populations can help eliminate a major source of transmission.
· Proper waste management. Properly disposing of animal and human waste can reduce breeding grounds for flies.
· Improved access to water. Having a fresh water source nearby can help improve hygienic conditions.
No trachoma vaccine is available, but prevention is possible. The World Health Organization (WHO) has developed a strategy to prevent trachoma, with the goal of eliminating it by 2020. The strategy, titled SAFE, involves:
· Surgery to treat advanced forms of trachoma
· Antibiotics to treat and prevent the infection
· Facial cleanliness
· Environmental improvements, particularly in water, sanitation and fly control
DIAGNOSIS
Trachoma disease is usually clinically diagnosed. People are examined for clinical signs through the use of magnifiers (loupes). In most early stages, infection does not present visible signs of the disease. However, repeated infections cause scarring of the conjunctiva and it is during this phase that infected individuals get the feeling of irritation.